Breathing Easy: A Nurse’s Guide to Conquering Seasonal Allergies

Are you among the more than 50 million people in the United States who identify the changing seasons by the number of tissues you need? Seasonal allergies are nothing to sneeze at—no pun intended.
Whether you're a nurse who is a seasonal allergy sufferer or someone who commiserates with those who are—this nurse's guide to conquering seasonal allergies is filled with helpful information on alleviating the nasty and uncomfortable symptoms that plague you or your colleagues and patients.
Understanding Seasonal Allergies
There are predictable increases in allergen counts during certain times of the year—mainly during the growing season when pollen and mold counts are high. Pollen and mold are the two most common seasonal culprits that trigger the immune system. Anyone sensitive to these allergens dreads the inevitable release of histamine—and the body's uncomfortable allergic response.
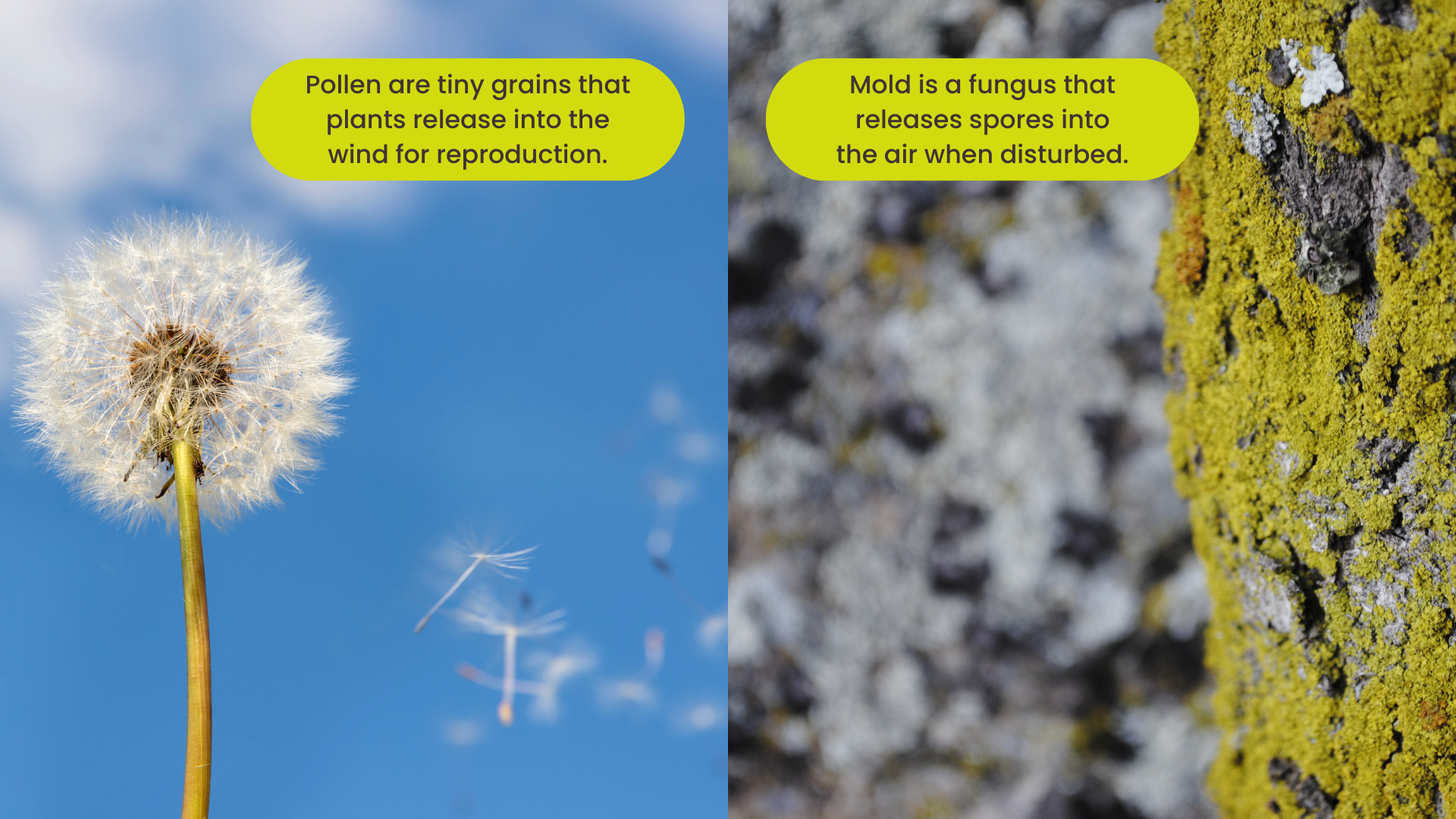
Pollen
Pollen are tiny grains about the size of a large dust particle that plants, such as trees, grasses, and weeds, release into the wind for reproduction. You'll find higher tree and grass pollen counts in the spring and higher weed pollen counts, such as ragweed, in the late summer and fall. Peak seasons differ depending on where you live.
Mold
Mold is a fungus that releases spores into the air when disturbed. A living organism, mold grows best in damp environments, such as basements, bathrooms, and rotting logs—and can be furry or flat and black, green, orange, or white. While mold grows year-round, there are more spores during spring and summer.
Is it Hay Fever or Allergic Rhinitis? Mold and pollen allergies share the same symptoms—known as seasonal allergies. This term is used interchangeably with seasonal allergic rhinitis—from the Greek word rhino, meaning nose—and hay fever, originating from farmers who suffered seasonal allergies when harvesting hay in the summer and fall.
Staying Ahead of Seasonal Allergies
Allergy seasons are getting longer, and pollen counts are increasing. The United States covers many geographical areas with different growing seasons—meaning that spring and fall happen at various times throughout the country.
Regularly referring to an interactive allergen map is a great way to stay ahead of seasonal allergies and minimize the nasty symptoms they bring. For example, you can
Avoid traveling to some regions of the country during peak allergy seasons.
Participate in indoor activities on days with high pollen and mold counts.
Exercise early when the morning dew weighs down the pollen, making it less airborne.
Take medications to reduce your symptoms before going outside.
Essential Allergy Management for Nurses
Nurses with allergies to pollen and mold face unique challenges in their work environments. After all, it’s tough to hide symptoms and perform your duties when you’re struggling with allergic symptoms.
Do you know which types of pollen and/or mold spores affect you the most? Knowing your allergen triggers is vital to preventing or minimizing the symptoms you experience.
Here are some strategies and tips for allergy management:
Check daily pollen and mold forecasts. When pollen counts are high, spend less time outside, close your windows, and turn on the air conditioner. Also, consider installing HEPA air filters in your home. You can reduce mold exposure by wearing an N95 mask and spending less time outside during high mold counts.
Reduce exposure at home and work. Regularly clean your work area to remove dust, pollen, and mold spores. Use a vacuum cleaner equipped with a HEPA filter and damp-wipe surfaces to prevent stirring allergens into the air. Reduce indoor mold exposure by increasing the airflow in your house, repairing any leaking pipes, and regularly inspecting and cleaning moist areas such as bathrooms, laundry rooms, and basements.
Wear eye protection like wraparound sunglasses or goggles to protect your eyes from airborne allergens while outside. Also, consider wearing a hat to prevent allergens from landing in your hair.
Stay hydrated and practice self-care. Drink plenty of water to help thin mucus secretions, making clearing your airways of allergens easier. Stress can exacerbate allergy symptoms, so activities like yoga and meditation can offer relief.
Practice long-term allergy management. Don’t slack on allergy medications prescribed or recommended by your healthcare provider, such as antihistamines, nasal sprays, and eye drops. Consider immunotherapy—allergy shots and pills you put under your tongue called sublingual immunotherapy (SLIT).
Natural Remedies for Seasonal Allergies Symptoms
If you suffer from seasonal allergies, have you ever considered some of these natural remedies for relieving your symptoms?
Get enough Vitamin C, a naturally occurring antihistamine, via a supplement or eating fruits and vegetables high in Vitamin C.
Try a nasal rinse to clear the mucus from your nose.
Drink hot fluids to help clear your nasal passages.
Many people think honey is a cure, but science doesn't support the premise. Since bees don't collect pollen from the primary allergen-producing plants, honey doesn't contain enough common allergens to provide any desensitization. In addition, when bees make honey, their digestive system changes the pollen protein, and your digestive system finishes any possible benefits.
Promote Allergy-Sensitive Healthcare Settings
Even if you don't suffer from allergies, you can help those who do by helping to create an allergy-sensitive healthcare setting. Avoid bringing pollen and mold spores to work by:
Showering and washing your hair before coming to work.
Not wearing a sweater that you've worn outdoors.
Drying your scrubs in a dryer instead of hanging them outdoors.
Not hugging or petting your dog after you've put on your scrubs.
Supporting Patients With Allergies
About 4.1 million patients visit doctors' offices and clinics to get relief from their allergies. Because allergic reactions are similar to respiratory illnesses, it’s sometimes difficult to differentiate between them.
Common allergy symptoms include:
Sneezing
Itchiness of the throat, nose, and eyes
Stuffy nose
Runny nose and eyes
Swollen eyes
Cough
Patients suffering from seasonal allergies don't typically have fevers, chills, body aches, and pains.
Determining Patterns
Ask questions about when the symptoms began and whether they’ve had them before. If so, how often and where do they occur? Are the symptoms more apparent when they are indoors or outdoors? Do they get stronger when cutting the grass or working in the garden?
Precursors to Asthma and Sinusitis
Seasonal allergies are sometimes linked to other health conditions, the most common being asthma. Asthma is a lung condition that causes the airways to swell and produce extra secretions, which leads to coughing, wheezing, and difficulty breathing. Allergies don’t cause asthma, but they can trigger an asthma response.
A second condition is sinusitis—inflammation of the sinuses. The nose is a passageway to four pairs of hollow spaces in the skull called sinuses. The tissues inside the nose and sinuses often swell when they come in contact with an allergen—which traps air and mucous and causes pain in the forehead and below the eyes. A virus, bacteria, or allergies can cause sinusitis.
Allergy Education and Awareness
Education is a primary responsibility of nurses in supporting patients with allergies. The knowledge you give your patients empowers them to take ownership of their health. Various ways to provide education are to give them fact sheets about allergens, teach them prevention tactics, and discuss the types of treatments and medications that may alleviate their symptoms.
Conclusion
Seasonal allergies can significantly impact the lives of nurses and their patients, often disrupting daily routines and causing discomfort. However, armed with knowledge and proactive measures, both nurses and patients can effectively manage and mitigate the symptoms associated with pollen and mold allergies.
By staying informed about allergen forecasts, implementing basic allergy management strategies, considering natural remedies, and promoting allergy-sensitive healthcare settings, nurses can alleviate their symptoms and provide better support and care for their patients.
Want the flexibility to work when, where, and how often you want? Download the ShiftMed nursing jobs app today!