How to Reduce Travel Labor With Data-Driven Healthcare Workforce Planning

Is your hospital's overreliance on travel nurses disrupting budgeting and forecasting, threatening financial stability and patient access? It may be time to move away from costly reactive contract labor and embrace a proactive healthcare workforce planning strategy driven by data.
3 Hidden Costs of Travel Nurse Dependence
In 2023, hospitals spent approximately $51.1 billion on contracted labor, highlighting their continued reliance on travel nurses to address staffing gaps.1 However, this dependence comes with significant costs that extend beyond the direct labor expenses and the price surges seen during emergency scenarios.
1. Lower Care Quality
Travel nurses' transient nature and unfamiliarity with specific healthcare settings can lead to missed cues, communication breakdowns, and suboptimal patient outcomes. A PubMed Central article from May 2024 examined the link between agency staffing and quality outcomes, finding that contract labor can negatively impact patient care. As quality declines, it doesn't go unnoticed—payers, providers, and patients take note, which can harm a hospital's reputation and long-term profitability.
2. Lower Staff Morale
Additionally, travel nurses often require closer supervision and may face challenges integrating into established team dynamics. The expectation for staff nurses to train travel nurses—who sometimes earn double their salary—can create tension and strain workplace relationships, disrupt patient care, and increase nurse turnover.
3. Less Control
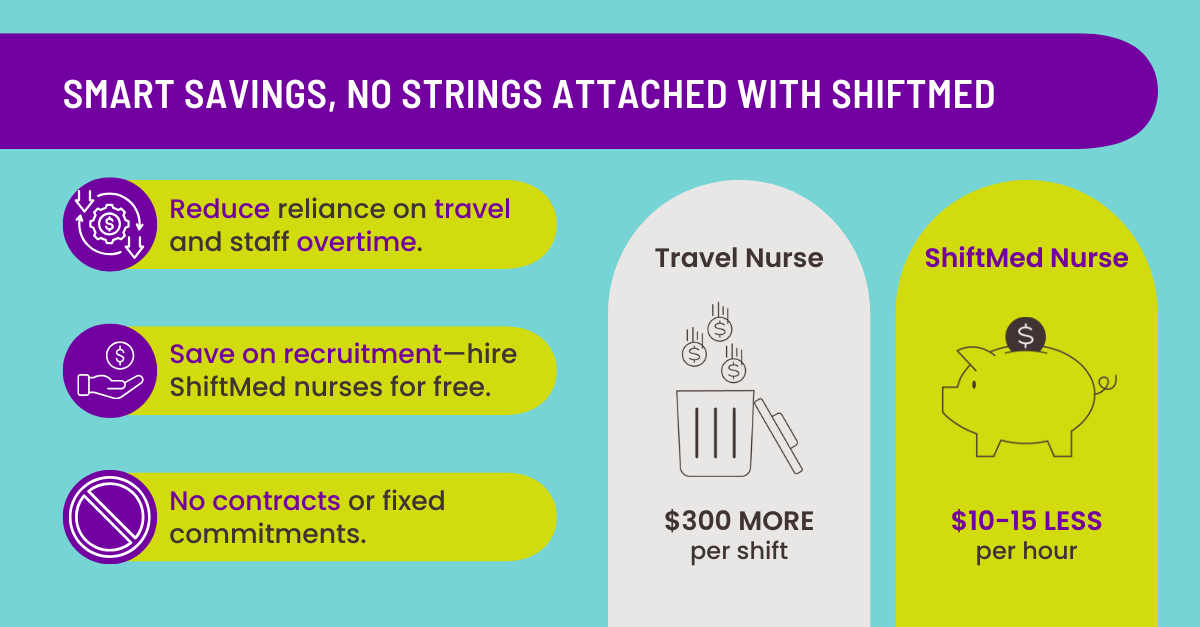
Relying on travel nurses places your hospital at the mercy of the agency that supplies them. These agencies maintain the contractual relationship with the nurses and often bind hospitals to 13-week contracts, which can result in unnecessary labor costs. For example, if patient demand decreases during the contract period, you may no longer need the additional staff—but you're still obligated to pay for them.
Reduce Travel Labor Today for a Sustainable Tomorrow
With nurse staffing shortages projected to persist, some reliance on external labor remains unavoidable.2 However, your hospital can still lower labor costs, maintain high-quality care, and promote workplace harmony by adopting a proactive healthcare workforce planning strategy. By leveraging a flexible staffing model and advanced workforce management technology—featuring AI-powered predictive nurse scheduling and healthcare staffing analytics—you can ensure efficient, coordinated care delivery.
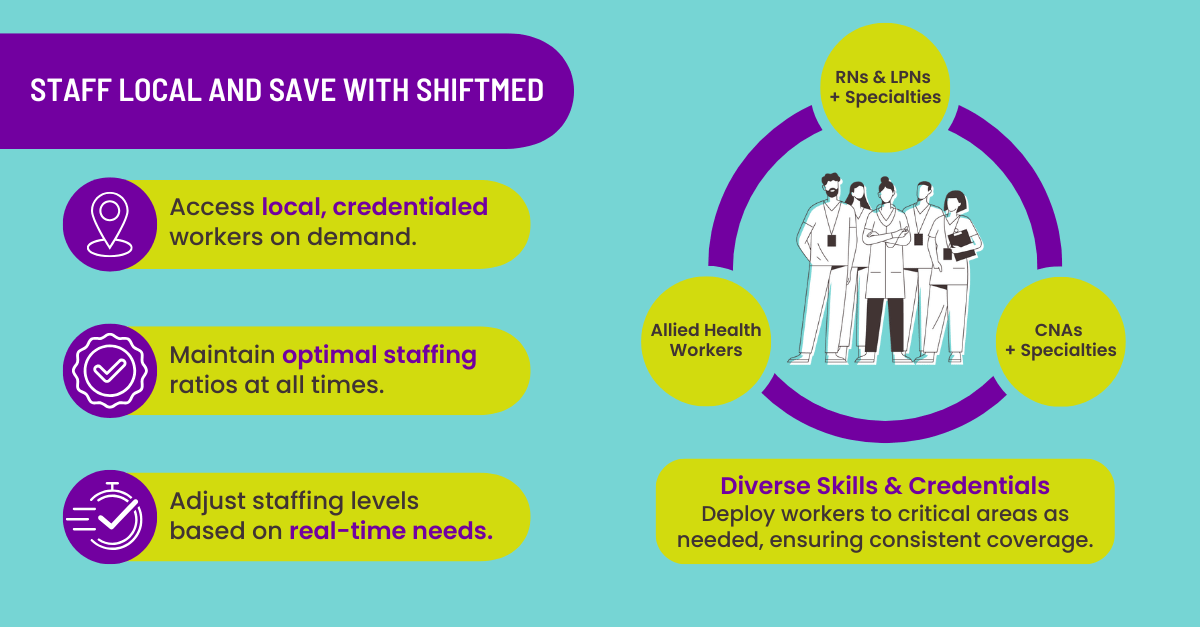
Flexible Staffing Models
A growing number of skilled nurses are seeking flexible, non-permanent positions within their local communities, allowing them to maintain stronger ties to their area compared to travel nurses. Nursing job apps like ShiftMed play a crucial role in making this possible, enabling hospitals to achieve stable, sustainable staffing levels by connecting them with local credentialed nurses seeking per diem work.
Predictive Nurse Scheduling
Nurse scheduling is a challenge for many hospitals. With the need to have enough staff at all hours, limited resources, and growing staffing shortages, the process can get tricky fast.
Nurse leaders are increasingly turning to predictive analytics to forecast patient demand months ahead, as reported by American Nurse Today. This approach eliminates guesswork in scheduling, giving leaders more time to focus on patient care and creating a better work environment for staff.
Furthermore, irregular shifts and uneven workloads can leave nurses feeling frustrated and patients feeling slighted in their care, proving that nurse scheduling optimization is vital to workforce well-being and a quality patient care experience.3 This makes predictive nurse scheduling a valuable tool in modern healthcare workforce management.
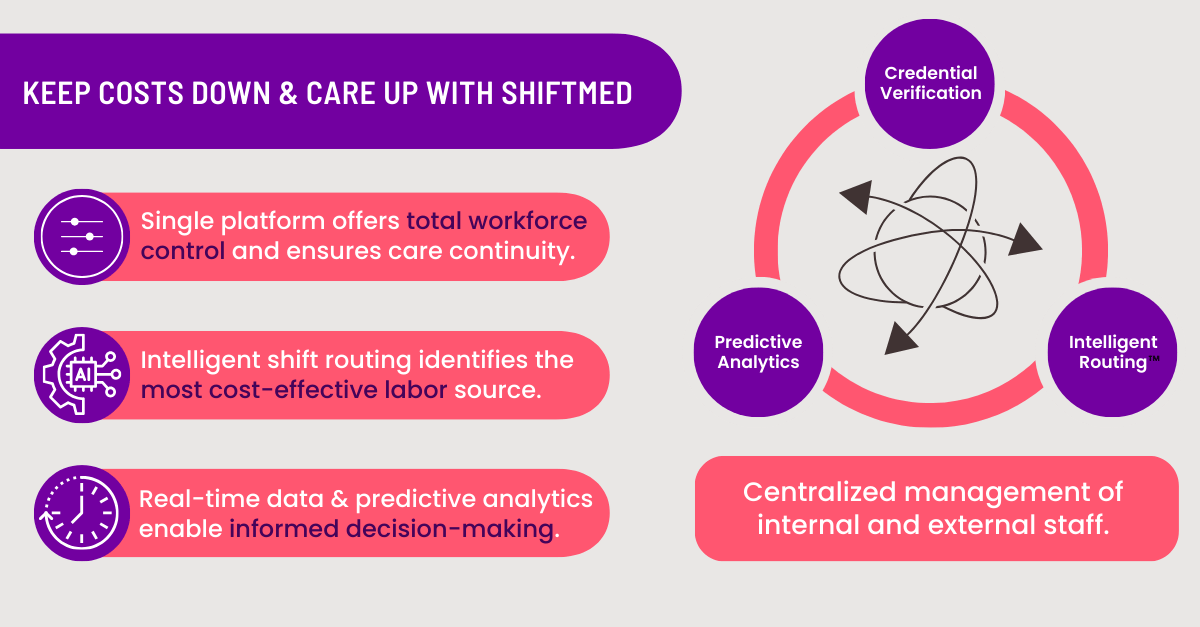
Predictive nurse scheduling is a component of healthcare staffing analytics. It uses historical data, seasonal trends, patient acuity, and staffing preferences to help hospitals plan, ensuring the right number of nurses with the right skills are scheduled at the right times to meet forecasted patient demand. This allows hospitals to boost operational efficiency, reduce costs, and satisfy staff and patients.
While predictive nurse scheduling excels at forecasting future needs, it also proves valuable in real time. For example, if the technology predicts an understaffed shift, schedulers can quickly identify and contact available nurses to fill the gap. Additionally, if a nurse calls out sick, the system automatically suggests a replacement based on current availability and skills, minimizing the time spent manually searching for coverage.
AI software is vital in predictive nurse scheduling and healthcare staffing analytics. It leverages data and advanced algorithms to optimize staffing decisions, reduce administrative burdens, and improve care quality.
Healthcare Staffing Analytics
More hospitals and health systems are starting to invest in healthcare staffing analytics to gain a comprehensive view of their workforce operations, including productivity, performance, and costs.
Hospitals and health systems must be agile enough to navigate the challenges of a rapidly changing and unpredictable world. Through technology, they can leverage analytics to enhance operations, streamline processes, and identify new opportunities or adapt their models to avoid potential disruptors.4
Consider that the healthcare industry generates massive amounts of data daily, from medical images and health records to financial reports. According to a 2020 AHA report, data production skyrocketed from 153 exabytes in 2013 to 2,314 exabytes in 2020. Transforming this data into actionable insights and integrating it into workflows can improve patient health, care quality, costs, transparency, staff morale, and satisfaction.4
5 Ways to Cultivate a Data-Driven Healthcare Workforce Strategy
Change is rarely easy for any organization and is incredibly challenging for legacy organizations. While these institutions often have a strong history of success, they must adapt to evolving business conditions and shifting consumer expectations to remain competitive.
A 2022 survey of global analytics leaders revealed that nearly 92% identified culture—not technology or employee expertise—as the biggest obstacle to becoming data-driven. Even the most advanced technology can fall short without a workplace culture that values and prioritizes data use.
Cultivating a data-driven workforce management strategy within your organization rests on five fundamental principles: 5
1. Leadership
Influential leaders understand the value of predictive analytics and actively promote data-driven decision-making throughout the organization. Appointing roles like a chief technology officer to champion these efforts can fast-track cultural change and inspire employees to embrace a data-driven mindset.
2. Data Accessibility
Data silos hinder collaboration, making data accessibility crucial for a successful workforce management strategy. However, unrestricted sharing can pose risks. Therefore, your organization must implement robust governance policies to protect data security while enabling authorized access for actionable insights and innovation.
3. Data Literacy
Employees must learn to access, interpret, and apply data to their roles. Providing targeted training emphasizes the value of data and equips workers to advocate for data-driven decision-making within their teams. Training should be continuous and evolve with organizational needs. Team leads should routinely evaluate departmental data fluency and refine skills as necessary.
4. Metrics
Workforce management success starts with identifying realistic goals and defining the desired outcomes. Your goals must be specific, measurable, achievable, and time-bound, with accountability assigned to critical stakeholders. You should also choose the right key performance indicators to support your goals.
For example, a KPI to track healthcare workforce management success could be "Staffing Efficiency Rate." This metric evaluates how effectively staffing levels align with patient demand and operational needs. You could also track "Cost Per Patient Day" by evaluating workforce-related costs against patient volume.
5. Continuous Commitment
Sustaining a data-driven culture requires ongoing effort and commitment. You can keep the momentum going by ensuring all data efforts support critical objectives, encouraging staff to consistently rely on data for decision-making, regularly reviewing and refining goals to ensure measurable outcomes, and investing in supporting technology that simplifies data access and makes insights readily available.
These foundational principles empower your organization to integrate data analytics seamlessly into your workforce management operations.
Conclusion
Optimizing hospital operations through data-driven healthcare workforce planning is no longer a luxury but a necessity in today's dynamic healthcare environment. The challenges of nurse staffing shortages, rising labor costs, and fluctuating patient needs require innovative solutions beyond reactive strategies.
Hospitals can enhance operational efficiency, reduce dependency on costly contract labor, and improve patient care quality by embracing predictive nurse scheduling, healthcare staffing analytics, and cultivating a data-driven culture.
Book a demo to see how ShiftMed workforce management solutions provide you with full oversight of your labor operations through predictive nurse scheduling, AI-powered software, and healthcare staff analytics.
Sources
1 American Hospital Association. 2024 Costs of Caring Report. 2024 April. https://www.aha.org/costsofcaring
2 Beauvais B, Pradhan R, Ramamonjiarivelo Z, Mileski M, Shanmugam R. When Agency Fails: An Analysis of the Association Between Hospital Agency Staffing and Quality Outcomes. Risk Manag Healthcare Policy. 2024 May 23;17:1361-1372. doi: 10.2147/RMHP.S459840. PMID: 38803621; PMCID: PMC11129761.
3 Abdalkareem, Z.A., Amir, A., Al-Betar, M.A. et al. Healthcare scheduling in optimization context: a review. Health Technol. 11, 445–469 (2021). https://doi.org/10.1007/s12553-021-00547-5
4 AHA Center for Health Innovation. Market Insights Report: Leveraging data for Health Care Innovation. 2021 January. https://www.aha.org/system/files/media/file/2021/01/MI_Leveraging_Data_Report.pdf
5 WebMD Ignite. 5 principles to creating a culture of data and analytics in healthcare. 2024 January. https://webmdignite.com/blog/5-principles-creating-culture-data-and-analytics-healthcare